State Prescription Drug Affordability Boards
What Are Prescription Drug Affordability Boards?
Prescription Drug Affordability Boards, also known as PDABs, are state government-appointed boards, or groups, that have the authority to review prescription drug costs and determine if they present an affordability challenge for patients. The intention of these boards, or PDABs, is to ensure that patients can get the medicines they need without having to pay too much money. These boards look at how much different medicines cost and decide if they are affordable for people.
More affordable drugs for patients sounds great, right? It does! We want affordable healthcare and treatment for all! But unfortunately, PDABs and the tools they use to measure affordability and fix “unaffordable” drugs aren’t providing cost savings to patients and are creating more barriers to accessing lifesaving drugs for patients.
Lack of Patient Engagement
PDABs are formed by policymakers and do not currently include patient, provider, or caregiver representatives who experience the real-world impact of treatments. Several already established PDABs have begun conducting reviews or selecting drugs to undergo affordability reviews – including in Colorado and Maryland – where patients have raised serious concerns about a lack of patient involvement throughout the process. Without a patient advocate or representative on the boards, any discussions or decisions made by that board are missing an imperative perspective and input. These groups should not be making these decisions without a patient representative.
Even when there are opportunities for patients to come to meetings to give their perspective and comments, these meetings are long and challenging to attend, sometimes announced with only 24 hours’ notice and are usually held during normal business hours when most are working. Surveys intended to collect patient feedback to determine whether a drug is affordable or not aren’t designed in a way that facilitates accurate responses, and any existing engagement processes feel designed only to check a box. To make matters worse, there is limited to no transparency in if and how PDABs are accounting for the feedback they receive from the patient community. Worst yet, is that if a patient is able to overcome these barriers and provide input or testimony to the boards, the patient input is not implemented or acted upon and no changes to the model or review are made.
What Are Upper Payment Limits?
Upper Payment Limits (UPLs) are a ceiling amount that a healthcare payer (e.g., Medicaid, commercial insurers) can reimburse for the purchase of a medication that a PDAB deems unaffordable. While it might seem like an easy fix, UPLs don’t actually impact what a patient pays out of pocket. The state, healthcare payors, etc. receive a lower cost but that cost savings does not trickle down to the patient.
In addition to not providing a patient benefit, UPLs also limit the amount that can be reimbursed to providers responsible for stocking, storing, and administering a treatment. The healthcare supply chain – getting a treatment from a research lab to the market for a patient to access – is incredibly complex and just one impact along the way threatens to interrupt the entirety of this delicate process. It already can take well over 12 years and billions of dollars to bring to new drugs to market. Because UPLs limit the reimbursement rate to manufacturers, this impacts the re-investment in innovation and research and could hinder and slow down future drug development.

Patients will face the hardest challenges because of UPLs. As companies in the supply chain try to control costs and protect their business, they might create barriers that make it harder for patients to get the treatments they need. Physicians could be deterred from prescribing certain drugs because of the lower reimbursement rates or drugs could become unavailable in states with UPLs on them altogether, forcing patients to face being prescribed drugs that are not best suited for them or having to travel across state lines to get their prescribed drugs. Both scenarios are unacceptable.

What is Quality-Adjusted Life Year?
A Quality-Adjusted Life Year (QALY) is a way to measure the value of medical treatments. It combines the length of time a person lives with the quality of their life during that time. One QALY equals one year of life in perfect health. For example, living two years with a condition that reduces your quality of life by half would equal one QALY.
This method of measuring treatments and quality of life are sometimes used by PDABs to determine if a UPL should implemented on a drug. In addition to the issues that can impact patients negatively that come with using UPLs, QALYs also cause concern in their use.
Everyone’s experience with illness and treatment is different. QALYs use averages that may not reflect individual patient needs and preferences and don’t capture the full impact of these conditions on a person’s life. QALYs can also oversimplify and overlook important aspects of personal health and well-being. Decisions about drug affordability should focus on what’s best for each patient.
Potential Impact of PDABs on Health Equity
PDABs increase access barriers without addressing financial barriers for patients. Instead of addressing patient costs, we’re likely to see higher hospitalization rates, and more emergency, acute care, and doctor’s visits, creating greater strain on patients and the health system overall as a result of PDABs and UPLs.
Black, Hispanic and Native Americans are up to two times more likely than white people to have major long-term conditions and are also more likely to forgo medical care due to cost with higher rates for Black folks delaying or forgoing treatments because of cost.

The drugs that were selected for an affordability review by the PDAB in Colorado (the only state to have conducted and concluded affordability reviews on the initial selected list of drugs thus far) were mostly treatments for chronic conditions, such as HIV and arthritis, which disproportionately impact Black patients.
If PDABs continue to select treatments for conditions that disproportionately impact communities of color to undergo affordability reviews, the already existing health gaps will continue to widen. The effects on health equity will be serious and long-lasting. If patients can’t get the treatments they need after being diagnosed with serious diseases—for example triple negative breast cancer (TNBC), metastatic breast cancer, and other diseases that disproportionately affect Black folks—the worst outcome could be death.

Tigerlily supports and advocates for efforts to make sure that drug prices are fair and reasonable, so that no patient has to choose between buying the medicine they need and other important things like food or rent. However, the current model being used for these PDABs is not that solution and we will continue to advocate for one where we can all win.
Let’s ensure the next generation gets access to cutting-edge, lifesaving and life sustaining treatments.


Currently eight states have enacted legislation to create a PDAB or similar entity to review the affordability of prescription drugs, four of which have the authority to set UPLs and just in 2024, twenty-four PDAB or “Affordability Review” related bills were introduced in twelve states.
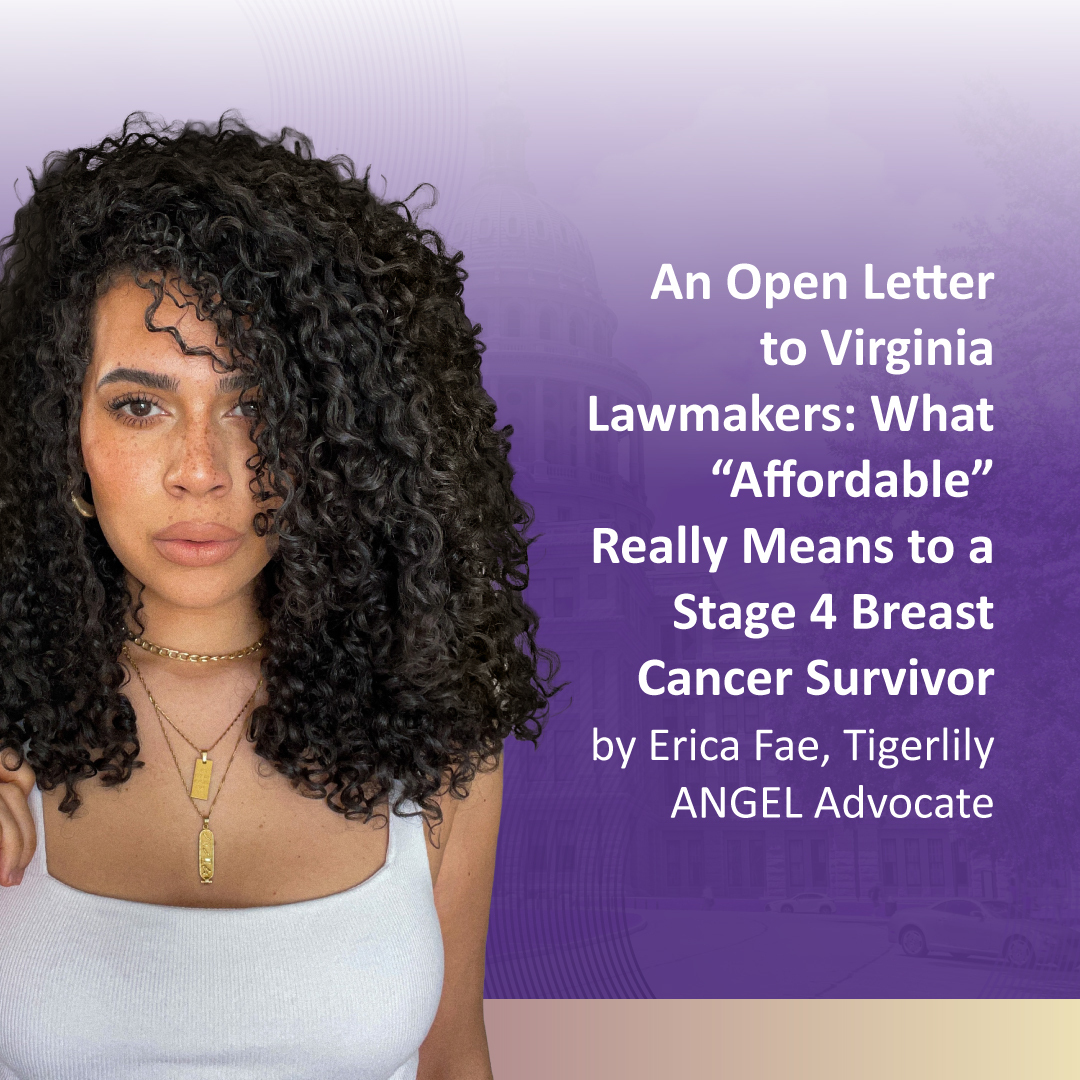
What does 'affordable' really mean?
PDABS Put Current & Future Cures for Virginians Out of Reach
Thank you to our sponsors
Transformational Sponsor
Inspirational Sponsor